Image powered by Unsplash
What pandemic mean to us:
The Spanish flu of 1918 infected an estimated 500 million people worldwide and killed an estimated 20 to 50 million victims, including some 675,000 Americans. One hundred years later, due to coronavirus, we seem to be revisiting this historical moment again. However, are we prepared to face this again and have we learned any lessons?
Why hospital capacity matter:
Of course the hospital capacity is not limited to the “number of beds“, or “number of ICU beds“. It is a total healthcare package of taking care of the patients, including the medical personnel, medical equipment (especially PPE and ventilators), and lastly the medical facility. However, it is also important to provide an isolated place for those has infected.
“Patients with risk factors for severe illness (see Risk Factors for Severe Illness above) should be monitored closely given the possible risk of progression to severe illness in the second week after symptom onset.”, according to CDC interim Clinical Guidance
The optimistic expectation of low mortality rate indicate there is higher chance of recovery after hospitalization. Isolate those patients before entering the severe illness state also help avoiding the disease spread.
Challenges for current medical facilities:
As the pandemic spreads and increases in scale many government and public health authorities are left scrambling because of the need to maximize patient beds for those infected. According to a recent USA Today health column, “the federal government has not publicly released estimates on demands COVID-19 might place on hospitals… if the pandemic worsens to levels of the 1918 Spanish flu pandemic, 2.9 million would need ICU care, according to the report.“
“One in seven cases require hospitalization and 5% require ICU care with ventilators to survive”. Yaneer Bar-Yam, a MIT-Trained physicist, also emphasized the urgency in his USA Today column.
As we see from the updated data, new cases (since 3/16/2020) increase exponentially and total active cases reached 82,300 in the United States, leaving a need of 11,700 beds nationwide.
Total Coronavirus Cases in the USA (as 3/25/2020), image excerpt from Worldmeters website
Daily New Cases in the USA (as 3/25/2020), image excerpt from Wordmeters website
What experts tells us:
Prefabricated element is a must solution for urgent demand
Prefabricated elements are particularly suitable for this urgent demand on healthcare facilities. Prefabricated units allow the construction of the foundation and the building envelope to take place in parallel. From having read about Wuhan’s Huoshenshan hospital being constructed in ten days, the construction industry has already brainstormed how quickly prefabricate these medical pods in order to meet the rapidly growing number of patients. Sean Studzinskiat at ModularDesign explained that pod-styled units which roll into larger spaces and lock into single story arrangements could come off the assembly line in as little as four to eight weeks.
Importance of Cohorting
Emergency medicine Physician Dr. Solomon Kuah, once helped the construction of a hospital during the 2014 Ebola outbreak in West Africa, mentioned the importance of “cohorting”- grouping people based on the level of risk. “You might have one wing where people confirm whether they have the virus and another where they are all tested positive.”
“They would also be divided from the main central areas by disinfection facilities, especially doctors are working across different group of patients” Dr. Kuah continued.
Limiting patient movement is a key
Reducing patient’s movement within the hospital will also help to ensure that risky individuals don’t come into contact with others. It is inevitable that infected patients will need to move, such as accessing toilets, reaching for nurse’s station, etc. Patient are admitted in different times and have different recovering cycle, thus causing different departure time from the hospital. In other words, limiting the operational transfer situation to avoid unnecessary contact will be the top priority.
One story structure is a preferred solution
“The half-lives of SARS-CoV-2 and SARS-CoV-1 were similar in aerosols, with median estimates of approximately 1.1 to 1.2 hours and 95% credible intervals of 0.64 to 2.64 for SARS-CoV-2 and 0.78 to 2.43 for SARS-CoV-1.“ A study from the New England Journal of Medicine reported.
“ When the virus becomes suspended in droplets smaller than five micrometers — known as aerosols — it can stay suspended for about a half-hour, before drifting down and settling on surfaces where it can linger for hours.” The New York Times.
Though an elevator could help speed up of the cohorting process (avoid long corridors) and reduce the built footprint as needed, an elevator is an enclosed space that has higher a chance of containing suspended droplets. If we heavily rely on elevators to transport patients to different zones, we would run into a higher chance of mixing high-risk individuals and not confirmed individuals together during elevator rides. (Even individuals checking in and out at different times, the droplets stay suspended in the elevator for about an hour. Therefore, place has less than three stories without hoistways’ ventilators could not meeting this criteria and could lead to more containment of coronavirus as compared to this possible alternative solution.)
Different need for semiprivate rooms
The standard shared toilet for four beds remains legislated in many state health codes: “One toilet room shall serve no more than two patient rooms and no more than four beds.” However, in this semiprivate (shared) room situation, an operational inefficiency and lower occupancy rate occurs because of the need for transferring male and female roommates to maintain same-sex occupancy.
A question for myself:
As we have seen this epidemic arrives in a bell curve to a specific region. New York Governor Andrew Cuomo warned that New York city is not a test case and urged other states take cautious actions.
"Look at us today... we are your future"… "New York is the canary in the coal mine, New York is happening first, what is happening to New York will happen to California and Illinois, it is just a matter of time". Governor Andrew Cuomo.
Shipping containers (ISO 8 ft wide, 8.5 ft high and come in three standard lengths, 10 ft, 20 ft and 40 ft)
Having spent the past two weeks in social isolation myself, I began to think about alternative uses for shipping containers that transport goods and products all over the world. Since there will be infrequent international travel during this period, many competing factors needed to be considered.
“Where are those places that best use of shipping container medical pods? ” I asked myself.
Ranking of ports in 2013 by trade volume. Ranking data from Wikipedia. Total COVID cases data from Worldmeters website.
There are still states that have COVID-19 active cases but do not have trade ports. Such as Arizona (401 cases) Utah (346) Nevada (405) Arkansas (280) District of Columbia (231 ) Iowa (145) Rhode Island (132) Kansas (126) New Mexico (112) Vermont (123) Idaho (91) Nebraska (64) Montana (53) North Dakota (45) South Dakota (41) Guam (37) Virgin Island (17) (source: www.worldmeters.info, updated 3/25/2020)
Side note:
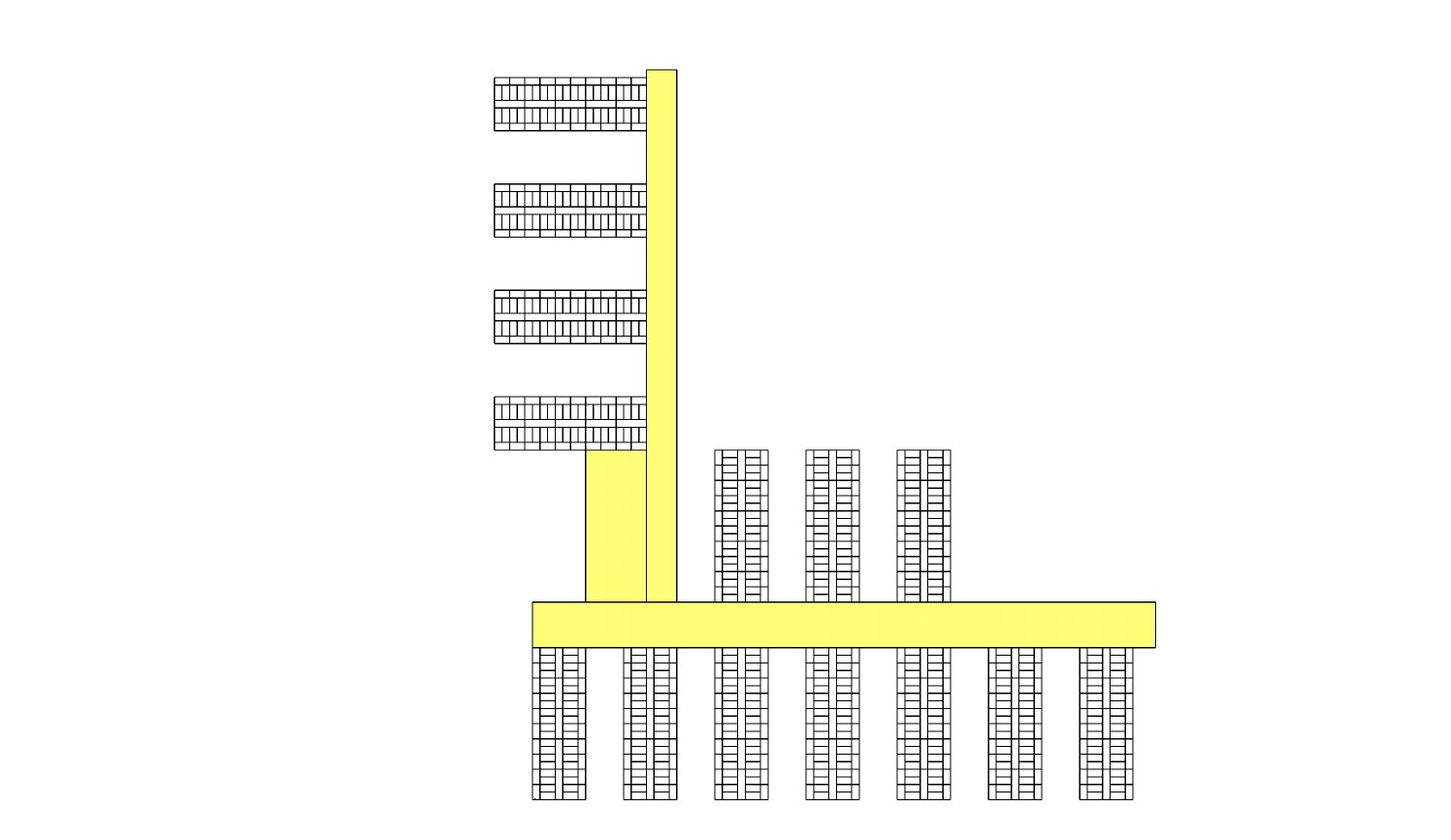
Here is an estimate of how many shipping containers would be needed to build a hospital of the size similar to Wuhan’s Huoshanshen Hospital.
Each wing would be composed by sixty-five shipping containers: five at the standard 40 feet, and sixty at the standard 20 feet. This configuration would provide forty rooms with 80 beds.
There are total fourteen wings on the site, which provides about 1120 beds (with total 840 of 20’ shipping containers for patient rooms and 70 of 40’ shipping containers to serve as corridor).
With all of the other administrative areas and medical worker stations, there would need to be an estimated 1430-1500 shipping containers for this size of hospital.
image excerpt from the web.
An illustration of how the shipping container works for Huoshanshen Hospital. The high lighted area are the restricted isolation system
Related readings:
“How to design a hospital that built in days, by someone who’s done it before”, CNN.com
“How Long Will Coronavirus Live on Surface or in Air Around You?“, The New York Times
“Coronavirus in the U.S: Latest Map and Cases Count“ The New York Times